If you are navigating the world of pain medication or dealing with addiction, you have probably heard the terms opioid and opiate used interchangeably. But here is the thing: they are not exactly the same, and understanding the difference between opioids and opiates can actually help you make better decisions about your health and recovery.
These powerful substances have helped millions manage severe pain, but they have also fueled a public health crisis that has touched countless families. Whether you are taking prescription opioids for chronic pain, worried about a loved one, or working through your own struggles with opioid use disorder, knowing what you are dealing with matters. This article breaks down everything you need to know about opiates vs opioids, how they affect your body, the risks involved, and, most importantly, what paths to recovery look like.
Quick Takeaways
- Opiates are natural substances derived directly from the opium poppy plant, while opioids include both natural and synthetic versions that interact with opioid receptors in your brain.
- Both opiates and opioids work by binding to opioid receptors in your central nervous system, blocking pain signals and creating feelings of euphoria that can lead to opioid addiction.
- Some prescription opioids are natural, some, like oxycodone, are semi-synthetic, and other drugs, like fentanyl, are fully synthetic opioids that can be 50 to 100 times stronger than morphine.
- Opioid use disorder is a recognized medical condition by the National Institute on Drug Abuse, and effective treatment options, including medication and therapy, are available.
- Physical dependence and tolerance develop quickly with regular use, leading to withdrawal symptoms that make quitting without help extremely difficult.
- Recovery is possible with the right support, whether through addiction medicine, mental health services administration programs, or peer support groups.
Understanding the Basic Terminology of Opioid Drugs
Let me clear up the confusion right away. When people talk about opioid vs opiate, they are usually referring to where these drugs come from. Opiates are the naturally occurring compounds extracted directly from the opium poppy plant. Think of commonly known compounds like morphine and codeine. These are the original pain relievers that humans have used for thousands of years. Your doctor might prescribe these for acute or chronic pain after a surgical procedure or injury.
Opioids, on the other hand, are the umbrella term that covers everything: natural opioids (opiates), semi-synthetic versions created by chemically modifying natural compounds, and fully synthetic drugs made entirely in laboratories. So while all opiates are opioids, not all opioids are opiates. The National Institute on Drug Abuse uses opioid as the catch-all term because it includes the entire family of these substances, whether they come from a poppy plant or a pharmaceutical lab.
Natural Opioids: The Original Pain Relievers
Natural opioids come straight from the opium poppy. Morphine is probably the most well-known opiate, and it remains one of the most effective medications for severe pain management in hospitals today. Codeine is another naturally derived compound often found in prescription cough syrups and mild pain medications. These substances have been around for centuries and work by mimicking the chemicals your body naturally produces to control pain. Recently, the Food and Drug Administration (FDA) has been restricting codeine, 2017 issuing its strongest warning against using codeine to treat children under the age of 12.
Semi-Synthetic Options: Modified for Medicine
Pharmaceutical companies take natural opioids and chemically alter them to create semi-synthetic versions. These modifications can make the drugs more potent, longer-lasting, or easier for your body to absorb. Common examples include oxycodone (found in OxyContin and Percocet), hydrocodone (in Vicodin), and hydromorphone. These prescription opioids became incredibly popular for treating chronic pain, but their potency also contributed to widespread opioid misuse and addiction.
Synthetic Opioids: Lab-Created Powerhouses
Synthetic opioids are manufactured entirely in laboratories through chemical processes and without using the opium poppy plant at all. Fentanyl is the most notorious example, and it is terrifyingly powerful. According to the National Institute on Drug Abuse, illicitly manufactured fentanyl has become a leading cause of drug overdose deaths because it is often mixed with other illegal drugs without users knowing. Although overdose death numbers sharply declined for the first time in decades during 2024, synthetic opioids like fentanyl remained the most significant driver of deaths. Other synthetic drugs in this category include methadone (used to treat opioid addiction) and tramadol.
How These Substances Affect Your Body
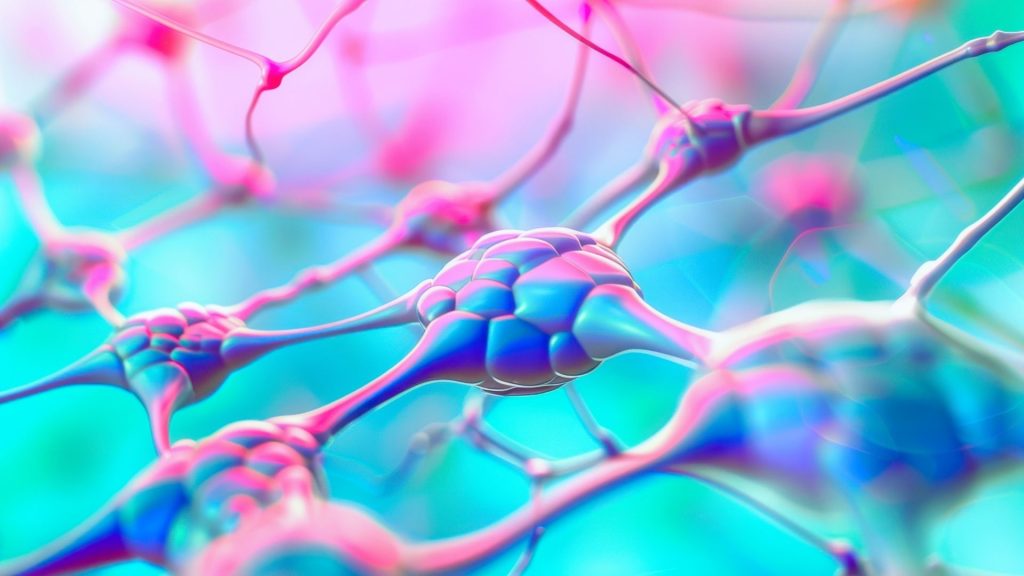
Whether you are taking opiates or opioids, they all work through the same basic mechanism in your body. They bind to specific opioid receptors scattered throughout your brain, spinal cord, and other areas of your central nervous system (CNS). These receptors are actually designed to respond to natural chemicals your body makes called endorphins. When you take an opioid drug, it floods these receptors with signals that block pain and trigger the release of dopamine, creating that sense of relief or even euphoria.
Here is what happens step by step: When you take the medication, it travels through your bloodstream to your brain. The drug molecules attach to opioid receptors on nerve cells, which stops those cells from sending pain signals to your brain. At the same time, this process activates your brain’s reward system, releasing dopamine and making you feel good. This is why opioids work so well for pain relief, but also why they are so addictive.
Opioid Strength Comparison (Oral administration):
| Drug Type | Relative Strength | Common uses |
| Codeine | 0.1x | Mild pain, cough |
| Tramadol | 0.1x | Moderate pain |
| Hydrocodone | 1x | Moderate to severe pain |
| Morphine | 1x | Severe pain (baseline) |
| Oxycodone | 1.5-2x | Severe pain |
| Hydromorphone | 5-10x | Severe pain |
| Fentanyl | 50-100x | Severe pain, anesthesia |
| Carfentanil | 10,000x | Large animal sedation only |
The Pain Relief Mechanism
Your body has a sophisticated system for managing pain signals. When you get injured, nerve cells send electrical signals through your spinal cord to your brain, where you perceive pain. Opioids interrupt this process at multiple points. They reduce the number of pain signals your nerves send, decrease how much your spinal cord transmits those signals, and change how your brain interprets whatever signals do get through. This is why they are so effective for treating acute injuries or helping people manage severe pain from conditions like cancer.
Building Tolerance and Dependence
Here is where things get complicated. Your body is incredibly adaptive, and when you take opioids regularly, it starts making adjustments. You develop tolerance, meaning you need higher doses to get the same effect. This happens because your brain reduces the number of opioid receptors or makes them less sensitive. Research shows this can happen within days or weeks of regular use.
Physical dependence is different from addiction, though they often occur together. Dependence means your body has adapted to having the drug present and will react badly if you suddenly stop. This leads to opioid withdrawal symptoms like muscle aches, nausea, anxiety, and intense cravings. These unpleasant symptoms drive many people to keep taking opioids just to avoid withdrawal symptoms, even when they want to quit.
The Reality of Opioid Addiction
It’s important to remember that opioid use disorder is not a moral failing or a lack of willpower on your part; it is instead best thought of as a complex brain disorder recognized by medical professionals and detailed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). When you have been taking opioids, your brain chemistry literally changes. The circuits involved in reward, motivation, and memory get rewired. What started as taking medication for chronic pain or an injury can evolve into a situation where you need the drug just to feel normal. This addiction gets compounded by the availability of illegal opioids sold on the streets. Substance use disorders fuel the trade of illicit drugs, which in turn increases the supply in a dangerous cycle.
Signs You Might Be Developing an Opioid Drug Abuse Problem
You might have opioid use disorder if you find yourself taking more than prescribed, spending excessive time obtaining or using opioids, continuing to use despite problems it causes in your life, or experiencing strong cravings.
- You might try to cut down, but find you cannot.
- Your work, relationships, or hobbies suffer because of your drug use.
- You take risks while under the influence or need increasing amounts to feel effects.
These are all warning signs that casual use has crossed into addiction territory.
The Overdose Crisis
Opioid overdose happens when you take more than your body can handle, causing respiratory depression, which can be life-threatening. Essentially, the drugs suppress your automatic breathing reflex to the point where you stop breathing altogether. This is life-threatening and requires immediate emergency response. The Centers for Disease Control tracks drug overdose deaths, and the numbers have skyrocketed with the introduction of illicitly manufactured fentanyl into illegal drug supplies over the past decades.
According to recent data from the National Center for Health Statistics, opioid overdose deaths have reached crisis levels. Synthetic opioid involvement in overdose death cases has increased dramatically because these substances are so potent that even tiny amounts can be fatal. Many people overdose without realizing their drugs contain fentanyl because dealers mix it into heroin, cocaine, and counterfeit pills. Law enforcement seized over 115 million pills containing illicit opioids containing fentanyl in 2023.
Getting Help and Treatment Options

If you are struggling, please know that effective treatment exists and recovery is absolutely possible. The field of addiction medicine has advanced significantly, and we now have multiple approaches that work. Treatment typically combines medication with behavioral therapy and support services, addressing both the physical and psychological aspects of opioid dependence.
Detox and Withdrawal Management
Going through opioid withdrawal symptoms without support is brutal and often leads to relapse. Medical detox programs provide a safe environment where health professionals can monitor you and provide medications to ease the worst symptoms. They can treat the nausea, help you sleep, manage anxiety, and keep you safe through the acute withdrawal phase, which typically lasts 5 to 10 days for short-acting opioids.
Medication-Assisted Treatment
Several medications can help treat opioid addiction. Methadone and buprenorphine are opioid drugs themselves, but they work differently from drugs of abuse. They satisfy your opioid receptors enough to prevent withdrawal symptoms and reduce cravings without causing the same high. This lets you stabilize your life while working on recovery. Naltrexone blocks opioid receptors entirely, preventing any opioid from having an effect if you relapse.
Therapy and Counseling
Medication helps with the physical aspects, but therapy addresses the underlying issues and teaches you new coping strategies. Cognitive-behavioral therapy helps you identify triggers and develop healthier responses. Group therapy provides a connection with others who understand what you are going through. Many people find tremendous value in peer support groups like Narcotics Anonymous, where you can share experiences and support each other through recovery.
Detox and Withdrawal Management
Going through opioid withdrawal symptoms without support is brutal and often leads to relapse. Medical detox programs provide a safe environment where health professionals can monitor you and provide medications to ease the worst symptoms. They can treat the nausea, help you sleep, manage anxiety, and keep you safe through the acute withdrawal phase, which typically lasts 5 to 10 days for short-acting opioids.
Prevention and Harm Reduction
For those currently using, harm reduction strategies can keep you safer while you work toward recovery. Carrying naloxone (Narcan) can reverse an overdose and save your life or someone else’s. Never use alone, so someone can call for help if needed. Test your drugs for fentanyl using test strips. These practical steps acknowledge that stopping immediately might not be realistic, but keeping yourself alive is the priority.
For Those Taking Prescription Opioids
If you are taking opioids for legitimate pain management, talk honestly with your medical provider about risks. Take medications exactly as prescribed and store them securely. Dispose of unused pills properly. Be alert for signs that you are developing tolerance or taking opioids more for emotional relief than pain relief. These are signals to have a conversation about alternative pain management strategies.
Preventing Opioid Misuse in the First Place
Disease control experts emphasize preventing opioid misuse before it starts. This means prescribers are being more judicious about when they prescribe opioids and for how long. It means exploring other approaches to treat pain, like physical therapy, non-opioid medications, and interventional procedures. It means education about risks and safe storage practices to prevent diversion to others.
Opioid vs Opiate Frequently Asked Questions
What is the difference between opioids and opiates?
The primary difference is their origin. Opiates are natural compounds extracted directly from the opium poppy plant, including morphine and codeine. Opioids are the broader term encompassing opiates plus semi-synthetic drugs made by modifying natural compounds and fully synthetic opioids created entirely in laboratories. Both interact with the same opioid receptors in your brain to block pain signals.
How quickly can someone develop opioid addiction?
Everyone’s risk differs based on genetics, mental health, dosage, and duration of use. Some people develop problematic use within weeks. Physical dependence can develop within days of regular use, causing withdrawal symptoms if stopped. Taking opioids exactly as your medical provider prescribes and monitoring for warning signs helps reduce risk.
Are synthetic opioids more dangerous than natural ones?
Synthetic opioids, particularly illicitly manufactured fentanyl, pose an extreme overdose risk because they are incredibly potent. Fentanyl is 50 to 100 times stronger than morphine, meaning tiny amounts can be fatal. However, any opioid drug carries risks of respiratory depression, addiction, and death when misused. The key difference is that synthetic drugs require much smaller doses to cause a life-threatening overdose.
What should I do if I think someone is overdosing?
Call emergency services immediately. Signs of opioid overdose include unconsciousness, slow or stopped breathing, blue lips or fingernails, and inability to wake the person. If you have naloxone, administer it right away following the product instructions. Naloxone temporarily reverses an overdose by blocking opioid receptors. Stay with the person, place them on their side, and perform rescue breathing if trained.
Moving Forward with Hope
Understanding the difference between opioids and opiates matters, but what matters more is recognizing that these substances, regardless of their origin, carry serious risks alongside their legitimate medical benefits. If you recognize yourself in this article, please reach out for help today.
You are not alone in this struggle, and you are not defined by your relationship with opioid drugs. Contact our admissions team at New Chapter Recovery if you or someone you love is struggling with opioid addiction. Our outpatient facility offers the best evidence-based, specialized care, with the flexibility to meet your life’s unique challenges.